Summary of Stroke Damage Reversed As Stem Cells Regrow the Brain:
Research from the University of Zurich demonstrates that stem cell therapy can reverse damage caused by strokes in mice, enabling neuron regeneration and restoring movement. With strokes affecting one in four adults, resulting in lasting impairments, the study aims to develop effective treatments for humans.
By transplanting human neural stem cells into mouses’ brains after a stroke simulation, researchers observed successful neuron formation and enhanced brain recovery processes, including improved blood vessel formation and reduced inflammation. Notably, the therapy showed better results when administered a week post-stroke.
While promising, the study emphasizes the necessity for safety measures and practicality in future human applications, such as developing an endovascular delivery method for the stem cells. Initial clinical trials for using induced stem cells to address Parkinson’s disease are already underway, with potential trials for stroke treatment to follow.
*****
Summary Bullet Points
- Stem Cell Breakthrough: Recent studies demonstrate that neural stem cells can regenerate brain tissue affected by strokes in mice, leading to significant recovery in movement and cognitive function.
- Mechanisms of Recovery: The research reveals that not only do these stem cells form new neurons, but they also promote other regenerative processes such as blood vessel formation and reduced inflammation.
- Clinical Implications: Insights gained from these studies point towards potential future applications in humans, with a focus on minimizing risks and simplifying treatment procedures.
- Timing of Treatment: Surprisingly, administering stem cells a week after a stroke may yield better outcomes than immediate treatment, providing a crucial window for preparation in clinical settings.
- Future Directions: Continued research is essential to ensure the safety of stem cell therapies, with initial clinical trials aimed at treating Parkinson’s disease already underway.
Stroke Damage Reversed: How Stem Cells Regrow the Brain
Imagine a world where strokes no longer carry the grim baggage of permanent disability. One in four adults may experience a stroke at some point in their lives, and tragically, approximately half will suffer lasting effects like paralysis or speech impairment. Strokes are largely caused by internal bleeding or insufficient oxygen supply, irreversibly damaging brain cells. The question that looms over this medical challenge is whether we can uncover therapies that catalyze recovery, effectively turning back the clock on brain damage. Recent breakthroughs in stem cell research offer a glimpse of hope.
The Groundbreaking Research
Christian Tackenberg and his team from the University of Zurich stand at the forefront of this exciting frontier. Their findings signal a promising advance towards healing the brain after a stroke. Through rigorous studies, they have demonstrated that neural stem cells—capable of regenerating various brain tissues—can flourish in a damaged brain and re-establish connections.
What a breakthrough this is! Imagine the implications: instead of accepting a fate marked by limited mobility or cognitive impairment, victims of strokes could regain functions that were thought to be lost forever. Tackenberg and postdoctoral researcher Rebecca Weber have collaborated with a team from the University of Southern California to peel back layers of complexity surrounding brain regeneration.
Entering the World of Neural Stem Cells
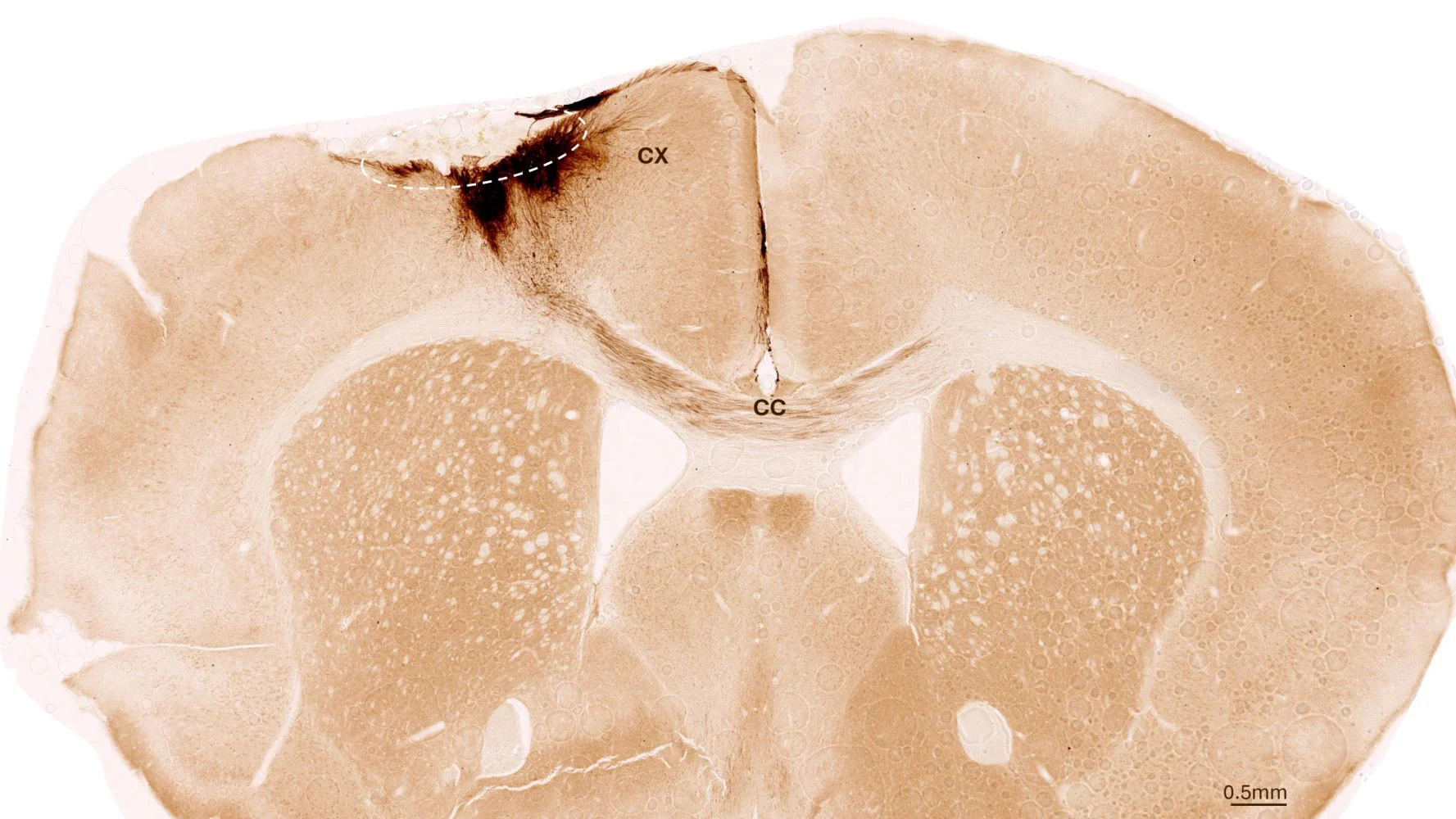
In their studies, researchers utilized human neural stem cells derived from induced pluripotent stem cells. These remarkable cells are generated from regular human somatic cells, providing a versatile source for various cell types. For their investigations, Tackenberg’s team induced a stroke-like condition in genetically modified mice, allowing them to accept the transplanted human stem cells without rejection.
Consider the beauty of this process: just a week after the stroke induction, these lab researchers introduced neural stem cells into the affected region of the mouse brain. Using a combination of imaging techniques and biochemical analyses, they observed remarkable changes over a five-week period. The results were nothing short of astonishing.
Unveiling the Recovery Mechanism
One of the key revelations from this study is that neural stem cells not only survived but thrived. Most of these cells transformed into functional neurons, establishing connections with the remaining healthy brain cells. It is as if nature whispered a message to these embryonic cells, encouraging them to thrive in an environment that was once devastated.
Moreover, the experiments revealed additional recovery markers: the formation of new blood vessels, a reduced inflammatory response, and improved integrity of the blood-brain barrier. Such regenerating processes extend far beyond forming new neurons, indicating a holistic approach to healing the brain’s complex environment.
Imagine this: you suffer a stroke, only to find that, a few weeks later, there’s a spark of new life where none existed before. Cells that once seemed hopelessly damaged are regrowing, reinforcing the intricate network that fuels thought, movement, and sensation.
Timing is Everything
Perhaps one of the study’s most unexpected insights is the timing of stem cell administration. In a world where every second counts, the researchers learned that administering these regenerative cells a week after the stroke could yield vastly superior outcomes compared to immediate treatment. This finding holds significant promise for streamlining therapeutic approaches, allowing healthcare providers ample time for preparation.
In an era where instant solutions are often glorified, it’s refreshing—and eye-opening—to realize that sometimes, waiting might indeed enhance potential outcomes. It incentivizes us to think less about haste and more about strategy.
Bridging Research and Clinical Application
Transitioning from mouse studies to human clinical trials is a daunting task. Tackenberg and his team are keenly aware of the need to minimize risks when developing therapies aimed at stroke recovery. They’ve devised a research protocol that eliminates the use of animal-derived reagents in stem cell manufacturing, making it safer and more applicable to human treatments.
Research and innovation require not only creativity but also dedication to ensure safety. Tackenberg is focused on establishing a safety switch to prevent the uncontrolled growth of stem cells post-transplant. Additionally, they are working on endovascular injection methods that could replace more invasive approaches like brain grafts. Imagine a future where treatment involves a procedure as routine as an endoscopy, all the while holding the promise of neurological regeneration.
The Road Ahead
Despite the remarkable strides being made, Tackenberg urges caution. “There is still work to be done,” he states. This statement resonates far beyond a simple acknowledgment of ongoing challenges. It serves as a reminder that while science is rapidly evolving, the journey to full-scale application in humans is complex.
Ongoing studies are crucial. The current initiatives include clinical trials exploring the potential of induced stem cells in treating conditions like Parkinson’s disease. If successful, stroke therapy could soon follow suit, transforming how we approach stained legacies left by neurological impairments.
A Reflection on Possibilities
This exploration into neural stem cell therapy is more than just a medical marvel; it’s a transformative concept that challenges our perception of recovery. It holds the potential to reshape not only medical protocols but also societal attitudes toward disabilities and stroke recovery. Just imagine how lives could change for stroke survivors and their families.
These advances beckon us to hold onto hope, to strive for resilience in the face of adversity. What if someday your loved ones, or even you, could emerge from such profound challenges renewed? Would it not inspire a newfound appreciation for our health and encourage us to advocate for research and therapies like these?
The Final Word: A Collective Encouragement
As you ponder the implications of this research, consider the larger narrative it contributes to: the journey of humanity facing insurmountable odds only to discover new avenues of healing and hope. The ongoing challenges may be myriad, but the strides being made are remarkable. Each breakthrough builds upon the last, collectively drawing us closer to a reality where stroke damage is a thing of the past.
So, let us embrace the journey. Let us be inspired by the courage and ingenuity of those pioneering the future of stroke recovery. The complexities of neuroscience may appear daunting, but in these scientific explorations lies the essence of what it means to move forward—together, we can elevate the narrative surrounding health recoveries and inspire new generations towards unyielding hope.
In conclusion, keep an eye on these developments in stem cell research. As science transforms possibility into reality, let us mirror that spirit of regeneration in our own lives—embracing new beginnings and celebrating every step toward healing.