Summary of “Sugar Hypothesis” of Diabetic Cataract Development Gets an Eye-Opening Reality Check:
New research challenges the long-held “sugar hypothesis” that high blood sugar precedes diabetic cataracts by suggesting that immune cells cause cellular changes in the eye lens before high blood sugar levels occur. The study by Brigham and Women’s Hospital discovered a novel mechanism that may bring the medical community closer to understanding diabetic complications’ origins and non-surgical treatments. Preclinical models showed that immune cells migrate from the eye’s ciliary bodies towards the lens, resulting in cellular changes before high blood sugar levels are present. The research team used an animal model that more closely recapitulates type 2 diabetes in humans.
*****
New findings challenge the “sugar hypothesis” in diabetic cataracts, revealing that immune cells cause cellular changes in the eye lens before high blood sugar levels occur. This suggests diabetic complications may begin during the pre-diabetic state and calls for reevaluating current theories.
Current Hypothesis Challenged
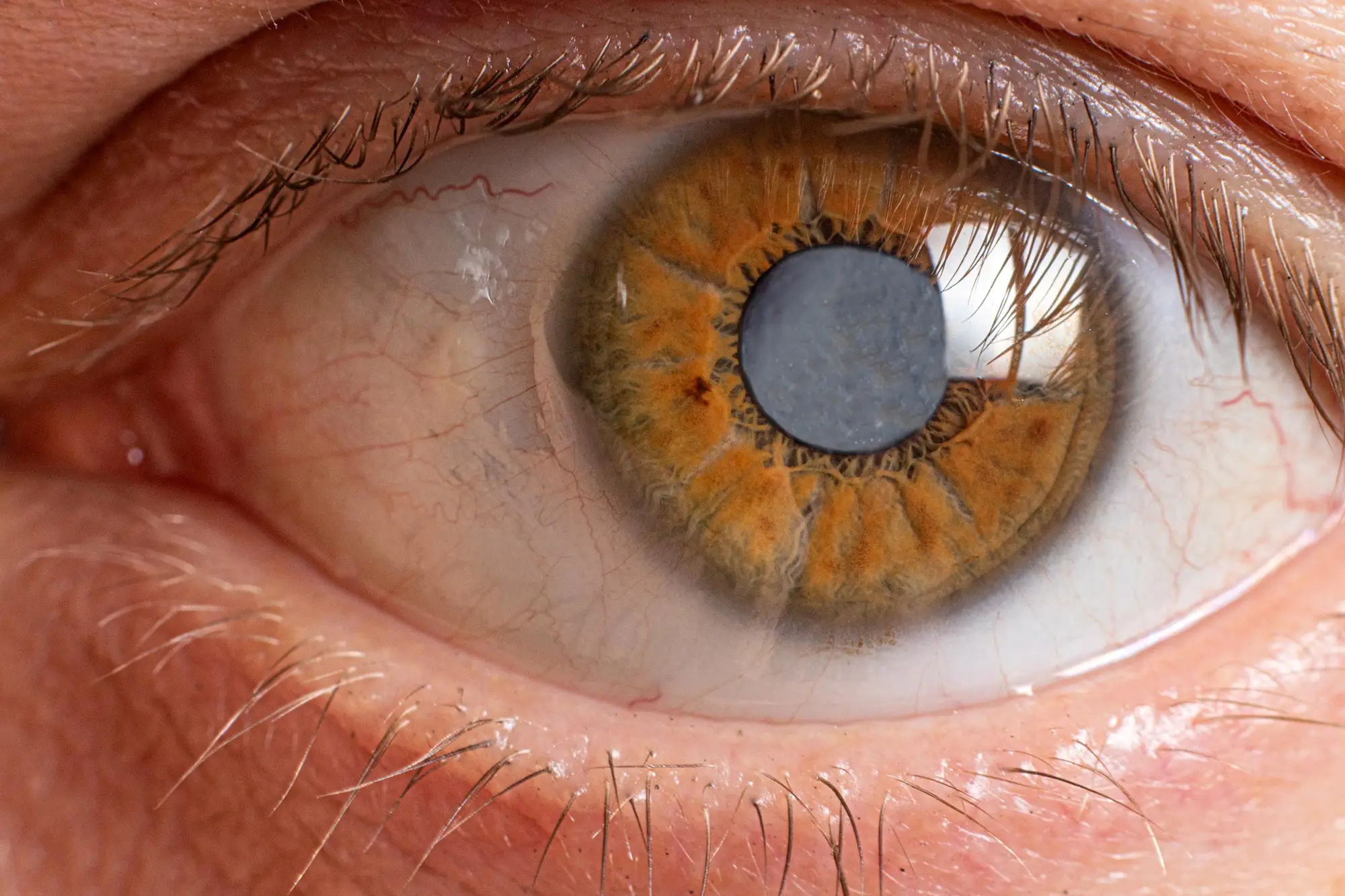
Cataracts, the clouding of the eye’s lens, are the number one cause of blindness worldwide and are a common complication of type 2 diabetes. The current hypothesis behind diabetic cataract development is “the sugar hypothesis,” which suggests that high blood sugar, a hallmark of diabetes, precedes cataract development. While unproven, researchers rarely investigate this theory further due to cataracts’ treatable nature.
Novel Mechanism Found
However, Brigham and Women’s Hospital researchers have discovered a novel mechanism in the development of diabetic cataracts, challenging the long-held “sugar hypothesis.” Their study revealed that immune cells migrate from the eye’s ciliary bodies towards the lens, resulting in cellular changes compromising lens function. These changes occur even before high blood sugar levels are present, suggesting that diabetic complications may begin during the pre-diabetic state.
New Preclinical Model Used
The research team used an animal model that more closely recapitulates type 2 diabetes in humans, the Nile grass rat, which spontaneously develops type 2 diabetes when kept in captivity and closely mimics the condition in humans. Using a specialized technique termed stereo microscopy with dual bright-field illumination, researchers observed the development of dot-like microlesions, which predisposed cataract formation in the inner cortical regions of the lens.
Immune Cell Trafficking Underlying Cataract Formation
Unexpectedly, researchers identified immune cells migrating from specialized structures in the eye called the ciliary bodies toward the lens. In these areas, where the immune cells traversed the capsule of the lens, they found that the epithelial cells that generally cover the inner surface of the tablet changed their identity and behaved differently. These changes also referred to as epithelial-mesenchymal transformation (EMT), were followed by seemingly unorganized cell growth, cell death, and cell migrations into the body of the lens.
Implications for Diabetic Complications
While still too early to tell what exactly causes the immune cells and epithelial cells to behave the way they do, the researchers conclude that their study urges further investigation of prevailing theories. It may also bring the medical community a step closer to understanding the cellular mechanisms underlying the origins of diabetic complications during the pre-diabetic stage of the disease.
Prevention of Cataracts
Once the pathogenesis of diabetic cataracts is understood, there may be ways to prevent people with diabetes from developing cataracts and potentially other complications elsewhere in the body. Surgery, the current treatment option for cataracts, comes with the risk of complications and is expensive for individuals and healthcare systems.
In conclusion, new fam and Women’s Hospital challfindings enge the “sugar hypothesis” of diabetic cataracts, revealing a novel mechanism underlying cataract formation that undermines current theories. The immune cells in the eye cause cellular changes to compromise lens function before high blood sugar levels occur, suggesting diabetic complications may begin during the pre-diabetic state. Further investigation into these mechanisms may lead to non-surgical preventative measures for diabetic cataracts and other complications.