Summary of Deadly Pancreatic Cancer Found To “Wire Itself” Into the Body’s Nerves:
Researchers at the Technical University of Munich have uncovered a mechanism by which pancreatic cancer cells hijack the nervous system for growth. They identified “pseudosynapses” that allow these cells to absorb the neurotransmitter glutamate, which promotes tumor growth. This process, resembling normal synaptic communication, causes calcium waves that drive tumor progression.
The team found increased levels of NMDA receptors in pancreatic tumors, which facilitate this glutamate uptake. Experiments showed that blocking these receptors slowed tumor growth and reduced metastasis in mice. The findings suggest that therapies targeting the interaction between the nervous system and tumors could offer new treatment options for pancreatic cancer and potentially other cancer types.
*****
Summary Bullet Points:
- Pancreatic cancer cells exploit the body’s nervous system by forming structures called pseudosynapses to promote growth.
- These pseudosynapses allow cancer cells to absorb glutamate, a neurotransmitter, fostering tumor development through calcium signaling.
- Research at the Technical University of Munich has unveiled the potential for new treatment avenues by blocking NMDA receptors on cancer cells.
- The phenomenon of neural invasion has long been associated with cancer aggressiveness, but the role of synapse-like structures is a novel finding.
- Future therapies may target the interactions between tumors and the nervous system, opening new pathways for combating cancer.
The Intriguing Interplay Between Pancreatic Cancer and the Nervous System
Few things are more elusive than the intricate ways in which cancer adapts and survives. Among the many forms of this relentless disease, pancreatic cancer stands as one of the most tenacious, known not just for its late diagnosis but for its remarkable ability to outwit the body’s defenses. Recent groundbreaking research reveals an unexpected ally contributing to its malignancy: our own nervous system.
Understanding the Deadly Dance
Pancreatic cancer has long puzzled scientists and physicians alike, primarily due to its insidious nature. Nearly 57,000 new cases are diagnosed yearly in the United States, and yet, the survival rate isn’t promising. Many patients succumb to the disease within the first year of diagnosis. This epidemic of loss prompts rigorous inquiries into the underlying mechanisms that propel pancreatic tumors’ aggressiveness.
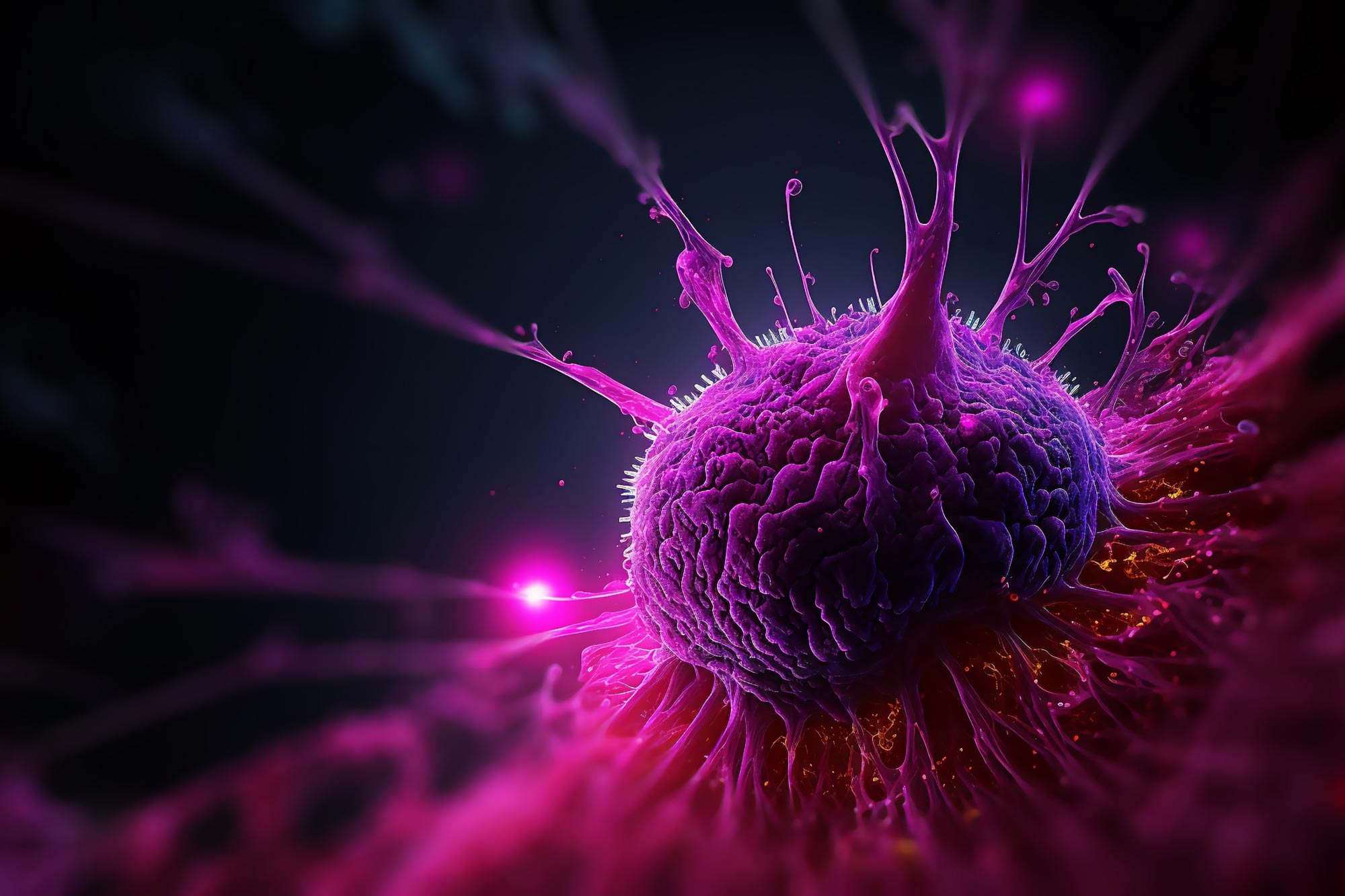
A recent study from the Technical University of Munich has opened a fascinating dialogue surrounding the interaction between pancreatic tumors and neural networks. They unveiled a unique method employed by cancer cells to hijack the nervous system, forming what the researchers have termed "pseudosynapses." These structures provide crucial support to the tumor, allowing it to flourish in a hostile biological environment.
The Science Behind Pseudosynapses
The term "pseudosynapses" may ring unfamiliar to many, but this innovation in scientific nomenclature accurately encapsulates a critical function. Typically, synapses facilitate communication between neurons by transmitting neurotransmitters from one cell to another, crucial for various processes, including movement, sensation, and emotions.
In pancreatic cancer cells, these pseud0synapses enable the tumor to absorb glutamate, a vital neurotransmitter involved in many neural processes, including the modulation of mood and memory. When glutamate binds to NMDA receptors on the cancer cells, it triggers an influx of calcium ions. This seemingly simple exchange sets off a cascade of signaling processes that enhance tumor growth and even metastasis—essentially creating a feedback loop of proliferation.
So why should you care? Knowledge of this mechanism could potentially transform treatment options for patients. The idea that a tumor can use a method normally reserved for neuronal communication is not only surprising; it opens the door to innovative therapeutic strategies that target this unique biological interface.
The Historical Context: Neural Invasion
To appreciate this new discovery, it is vital to contextualize it within the broader history of cancer research. Neural invasion—the phenomenon where nerve fibers infiltrate tumors—has long been associated with poorer outcomes. This relationship between tumors and nearby nerves has historically emphasized the aggressiveness of certain types of cancer.
Yet, the revelation that tumors can create their own synapse-like structures pushes the boundaries of our understanding. In a way, this discovery suggests that tumors are not solely passive entities but active participants in their own survival, employing a cunning and sophisticated method of exploitation.
Calcium Waves: A Tumor’s Secret Weapon
The question arises: why is calcium so influential in this context? When calcium enters cancer cells through NMDA receptor channels, it initiates a series of cellular signals that promote rapid proliferation and survival. The research team observed that pancreatic cancer cells generate what are known as "calcium waves." These slow, sustained oscillations in calcium concentration within the cells act as facilitators, further optimizing conditions for tumor growth.
The biology here is both complex and astonishing. It demonstrates how interconnected elements of our physiology can inadvertently assist malignancies. The fact that pancreatic tumors can modulate their own growth through elements typically associated with nerve signaling exemplifies an intricate game of survival that has far-reaching implications.
A Hopeful Future: Targeting Pseudosynapses
With the unveiling of these pseud0synapses, researchers are eager to explore potential avenues for therapeutic intervention. During their investigations, the team at TUM successfully blocked NMDA receptors on the cancer cells in mouse models. The results were promising: the pancreatic tumors exhibited slower growth rates, reduced metastatic potential, and notably, improved survival times for the animals.
In light of these findings, scientists are increasingly optimistic that targeting the NMDA receptor interface could yield new treatment options, not only for pancreatic cancer but potentially for other types of tumors that exploit similar mechanisms. The search for approved drugs that might act on these receptors is currently underway, showcasing an interdisciplinary approach to problem-solving in medicine.
The Ripple Effect: Implications Beyond Pancreatic Cancer
But here’s the kicker: this newfound knowledge doesn’t only pertain to pancreatic cancer. The notion that tumors might leverage neural signaling could extend to various cancer types. What if breast cancer or prostate cancer employs a similar tactic? The possibility invites us to rethink our strategies for diagnosis and treatment across the oncology landscape.
Understanding and Empowering Patients
As the research community delves deeper into these findings, the importance of engaging patients becomes critical. Knowledge is power; understanding the interplay between nervous system signaling and tumor behavior empowers patients in their journey. They’ll be more informed during consultations, more engaged in treatment decisions, and ultimately more proactive in their health management.
This dialogue isn’t solely academic; it’s personal. For those facing a cancer diagnosis, each shred of insight translates into hope. The discovery of new mechanisms provides not just medical pathways to explore but also psychological resources. Knowledge fosters resilience, equipping patients to navigate the often-arduous road ahead.
Final Thoughts: A Call to Action
The dialogue between pancreatic cancer and the nervous system exemplifies both the challenges and triumphs of modern medical research. As discoveries continue to unfold, it’s essential to remind ourselves—progress isn’t merely measured in clinical trials and laboratory results. It’s also reflected in the stories of patients, their strength, and their enduring hope.
The mission extends beyond individual survival; it’s a collective quest to shift terminal diagnoses into manageable conditions. Armed with innovative approaches to treatment and rich, appetizing discourse surrounding their implications, we can transform despair into a renewed sense of purpose and community.
In closing, as we stand at the intersection of human resilience and advanced medical insight, let this discussion remind us to confront the unknown with curiosity, to foster compassion in the face of adversity, and to celebrate every ounce of progress that reshapes our understanding of seemingly insurmountable challenges. Together, through shared knowledge and innovation, we can work towards dismantling the most formidable adversaries in the realm of health.