Summary of Clearing Toxic Waste Linked to Alzheimer’s – Study Finds Game-Changing Way To Boost Brain Immune Cells:
Researchers at Nanyang Technological University in Singapore have discovered a “metabolic switch” in the brain’s immune cells, which could be a target for Alzheimer’s disease treatment. By blocking and deactivating the switch, microglial immune cells in the brain were able to remove toxic proteins that can build up and lead to Alzheimer’s disease. The researchers hope to develop drugs that can specifically target metabolism in brain immune cells for Alzheimer’s disease. The findings were published in Proceedings of the National Academy of Sciences on 14 February 2023.
*****
“Metabolic switch” in brain immune cells could be key to Alzheimer’s treatment.
Currently, there are no definitive cures for the condition, which impairs people’s ability to think and is the most widespread form of dementia. Singapore researchers have discovered an “energy switch” in immune cells in the brain that could hold the key to developing drugs to treat Alzheimer’s disease. Scientists at Nanyang Technological University found that the microglial immune cells in the brain could remove toxic proteins which accumulate and cause Alzheimer’s when a key enzyme is blocked.
Discovery of “metabolic switch” in immune cells in the brain
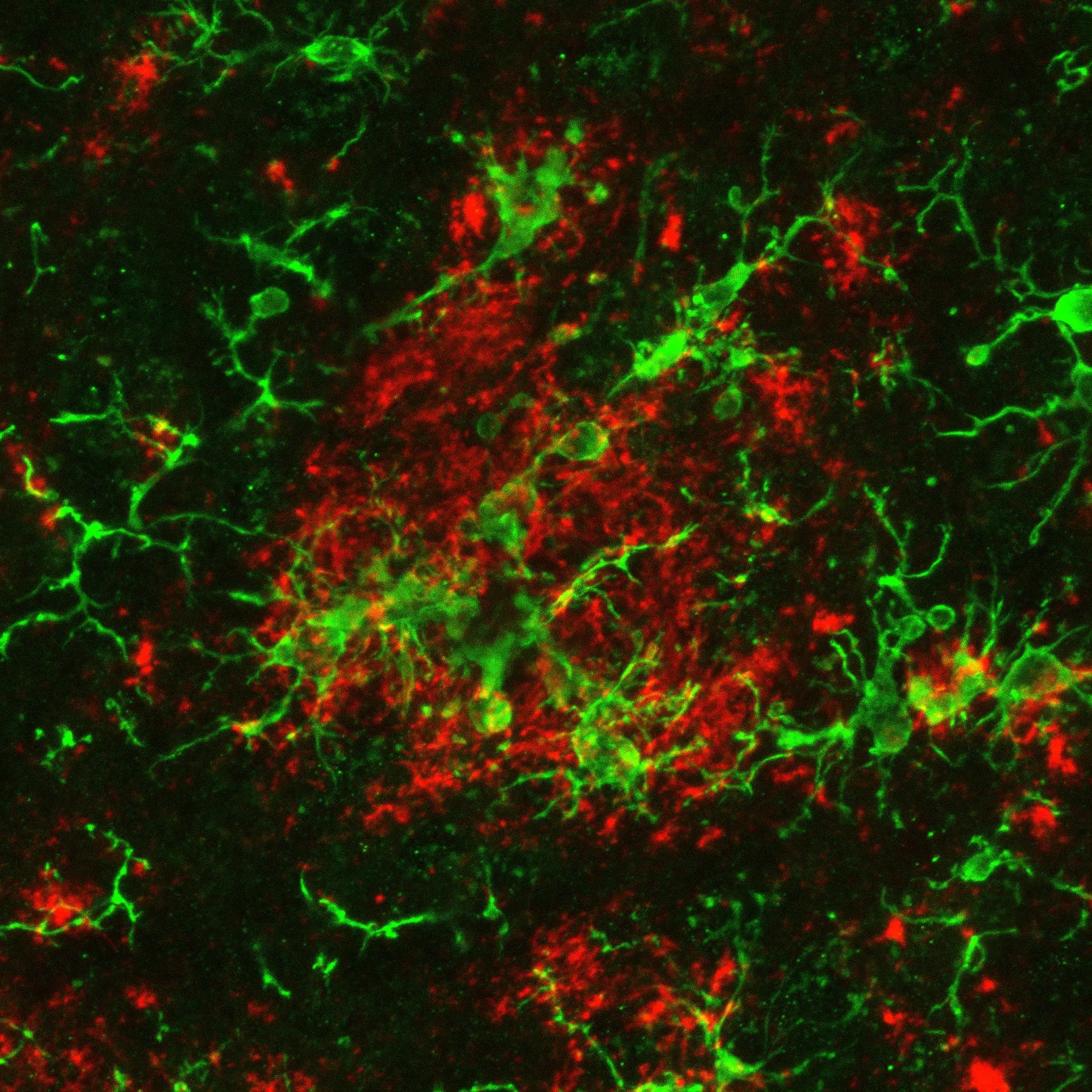
Microglia immune cells in the brain tend to be damaged in people with Alzheimer’s, making them less effective in clearing toxic cell waste. To restore the clean-up function, researchers “switched off” their inefficient metabolism by preventing a key enzyme from attaching to energy-generating parts of the immune cells. Such drugs are highly interested in healthcare as the World Health Organization estimates that 78 million people worldwide will have dementia by 2030.
Understanding the function of a biomolecule called the translocator protein
The researchers’ findings stem from their work investigating the function of a biomolecule called the translocator protein, which is found in energy-generating parts of immune cells. Asst Prof Anna Barron’s group had previously shown that drugs that activated the protein led to a less toxic waste build-up in the brain, which improved the condition of Alzheimer’s disease. Their latest experiments on cells from mice with Alzheimer’s showed that without the translocator protein, microglia immune cells of the brain had an energy problem and could not remove beta-amyloid, which worsened the disease.
The hexokinase-2 enzyme, which metabolizes sugar
The team developed a light-activated tool to manipulate the enzyme’s role in microglia energy production. When the translocator protein was absent, an enzyme called hexokinase-2 metabolized sugar to promote an inefficient way for microglia cells to produce energy. The researchers found that hexokinase-2 was also activated in microglia when exposed to more toxic forms of beta-amyloid. The scientists’ approach holds promise for studying cell energy production for other diseases and conditions, including diabetes and obesity.
Development of new drugs
Asst Prof Barron’s team’s findings provide for developing drugs that could act specifically on the metabolism of immune cells in the brain to treat Alzheimer’s disease. Such medications could prompt the brain’s microglia to produce energy more efficiently and thus clear toxic beta-amyloid proteins. As the strategy of hexokinase-2 displacement represents a potential therapeutic target for improved beta-amyloid removal by the microglia, the displacement of hexokinase-2 led to improved energy production. It enhanced the microglia’s ability to get rid of beta-amyloid.