Summary of Glioblastoma Therapy Doubles Down on Tumor Destruction:
Scientists at the University Health Network in Toronto have developed a therapy for glioblastoma that combines an oncolytic virus injection into the tumor with intravenous immunotherapy. The innovative treatment offers a “double hit” to tumors causing direct cancer cell death and stimulating local immune activity, leaving the cancer cells vulnerable to targeted immunotherapy. The Phase 1/2 clinical trial demonstrated that the treatment is safe and effective, producing evidence of prolonged survival in select patients. At the same time, researchers also found a genetic signature that could predict those most likely to respond.
*****
Combination of Oncolytic Virus and Anti-PD-1 Antibody Shows Promise in Fighting Glioblastoma
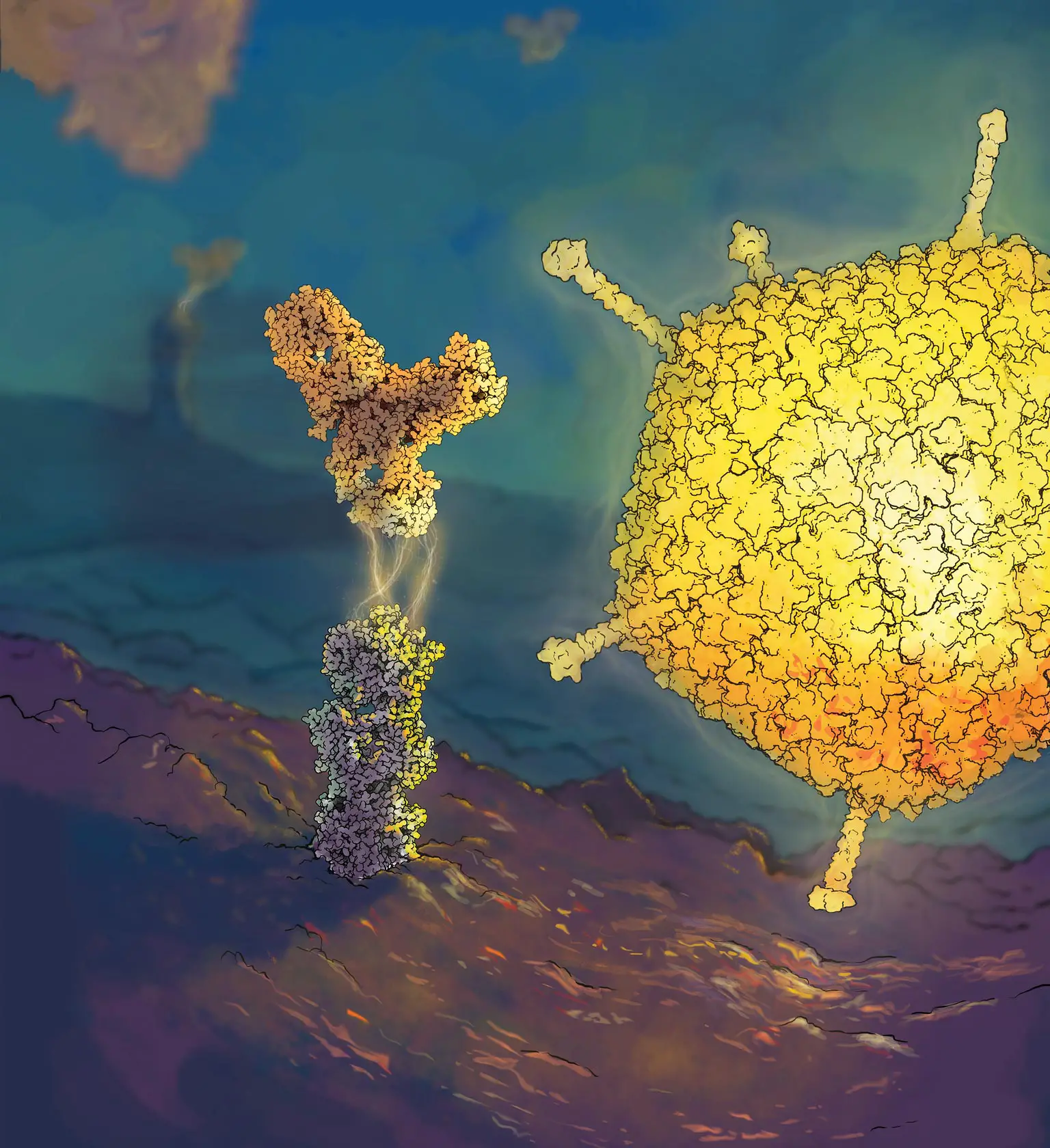
Researchers at the University Health Network in Toronto have published the results of a Phase 1/2 clinical trial for a promising new therapy for glioblastoma, a difficult-to-treat primary brain cancer. The treatment combines the injection of an oncolytic virus directly into the tumor with intravenous immunotherapy, using an anti-PD-1 antibody as a targeted immunotherapy.
The team injected the virus through a small hole and a purpose-built catheter, accurately localizing the tumor using stereotactic techniques. Patients then received an anti-PD-1 antibody intravenously every three weeks, starting one week after surgery. The combination of the oncolytic virus and immune-checkpoint inhibition results in a “double hit” to tumors; the virus directly causes cancer cell death and stimulates local immune activity, causing inflammation, making the cancer cells more vulnerable to targeted immunotherapy.
The study’s results, published in Nature Medicine, reveal that this combination therapy is safe, well-tolerated, and prolongs patient survival. The treatment had no significant unexpected adverse effects and yielded a median survival of 12.5 months, double that typically seen with existing therapies. This trial would not have been possible without the involvement of research safety teams, OR teams, and researchers, indicated Dr. Gelareh Zadeh, a senior author of the study.
The team also performed experiments to define mutations, gene expression, and immune features of each patient’s tumor and discovered vital resistant features that could eventually help clinicians predict patient treatment responses and understand the mechanisms of glioblastoma resistance.
The authors found that this novel combination therapy can eradicate the tumor in select patients, with evidence of prolonged survival. Investigative work by the authors revealed a new genetic signature within tumor samples that has the potential to predict which patients with glioblastoma are most likely to respond to treatment.
Furthermore, the therapy offers a promising “double hit” against cancer cells by causing direct cancer cell death and stimulating local immune activity, making the cancer cells more vulnerable to targeted immunotherapy. These results are significant as the patients in the trial only received injections of the virus, rather than resection, as a novel treatment approach for glioblastoma.
Moving forward, the group intends to test the effectiveness of the combination therapy against other treatments in a randomized clinical trial to continue the development of personalized treatments for glioblastoma. The trial’s findings are encouraging and demonstrate how translational work combining basic bench science and clinical trials can move personalized treatments for glioblastoma forward.