Summary of Cornell Scientists Uncover Major Mechanism Behind Lung Cancer’s Immune Evasion:
Researchers at Weill Cornell Medicine have found that a protein prevalent in high quantities within lung cancer cells, XBP1s, regulates a critical immunosuppressive pathway, enabling lung tumors to avoid immune response. This discovery could accelerate the creation of treatments aimed at overcoming this tumor defense mechanism, ultimately enhancing the prospects for lung cancer patients. The researchers demonstrated that XBP1s achieves this by promoting the production of the potent immunosuppressive molecule, prostaglandin E2. They suggest that disabling IRE1α-XBP1s might be a good treatment strategy for non-small-cell lung cancer, and could work particularly well in combination with other immunotherapy approaches.
*****
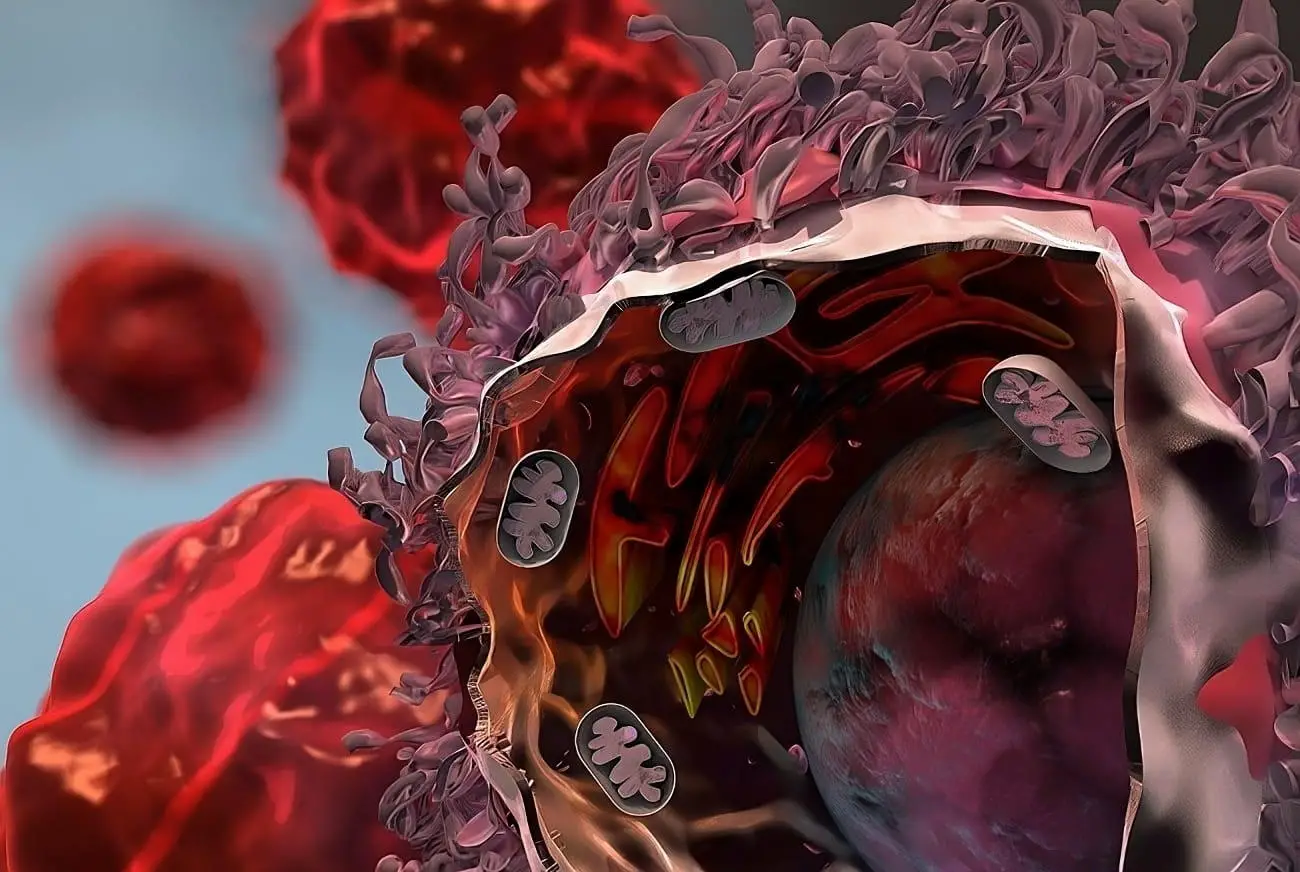
Lung Cancer Cells Use Protein to Suppress Immune Response
According to a study led by researchers at Weill Cornell Medicine, a protein prevalent in high quantities within lung cancer cells has been found to regulate a critical immunosuppressive pathway, enabling lung tumors to avoid immune response. This discovery could accelerate the creation of treatments aimed at overcoming this tumor defense mechanism, ultimately enhancing the prospects for lung cancer patients.
Uncovering the Role of XBP1s
The researchers, in their study published in the journal Nature Communications, analyzed datasets of human lung cancer and conducted experiments on preclinical models of lung cancer to demonstrate that the transcription factor XBP1s improves tumor survival by surpressing the anti-cancer abilities of neighboring immune cells. Through their investigation, they uncovered that XBP1s achieves this by promoting the production of the potent immunosuppressive molecule, prostaglandin E2.
Lung Cancer: The Leading Cause of Cancer Mortality
There are nearly 250,000 new cases of lung cancer every year in the United States, and more than 130,000 lung cancer deaths, according to the American Cancer Society, making this form of cancer the leading cause of cancer mortality in the country. The vast majority of cases are of a type called non-small-cell lung cancer (NSCLC), which is often diagnosed at an advanced stage of progression.
Newer Treatments Show Limited Success Against NSCLC
Newer treatments that attempt to dismantle cancers’ immune-suppressing defenses or attack tumors with engineered immune cells have shown promise against other cancer types but have had very limited success against NSCLC. Cancer researchers believe that this is due to NSCLC’s additional, undiscovered immune-suppressing mechanisms. Much research now is aimed at uncovering and finding ways to dismantle these additional regulatory pathways.
Disabling IRE1α-XBP1s Could Represent a Useful Therapeutic Approach
In the study, the researchers focused on the IRE1α-XBP1 arm of the unfolded protein response, a pathway that is chronically upregulated in many cancers. Prior studies of other tumor types have found evidence that this pathway not only directly promotes the survival and progression of tumors but also helps to suppress the antitumor activity of nearby immune cells. Yet the pathway’s role in NSCLC remained largely unexplored.
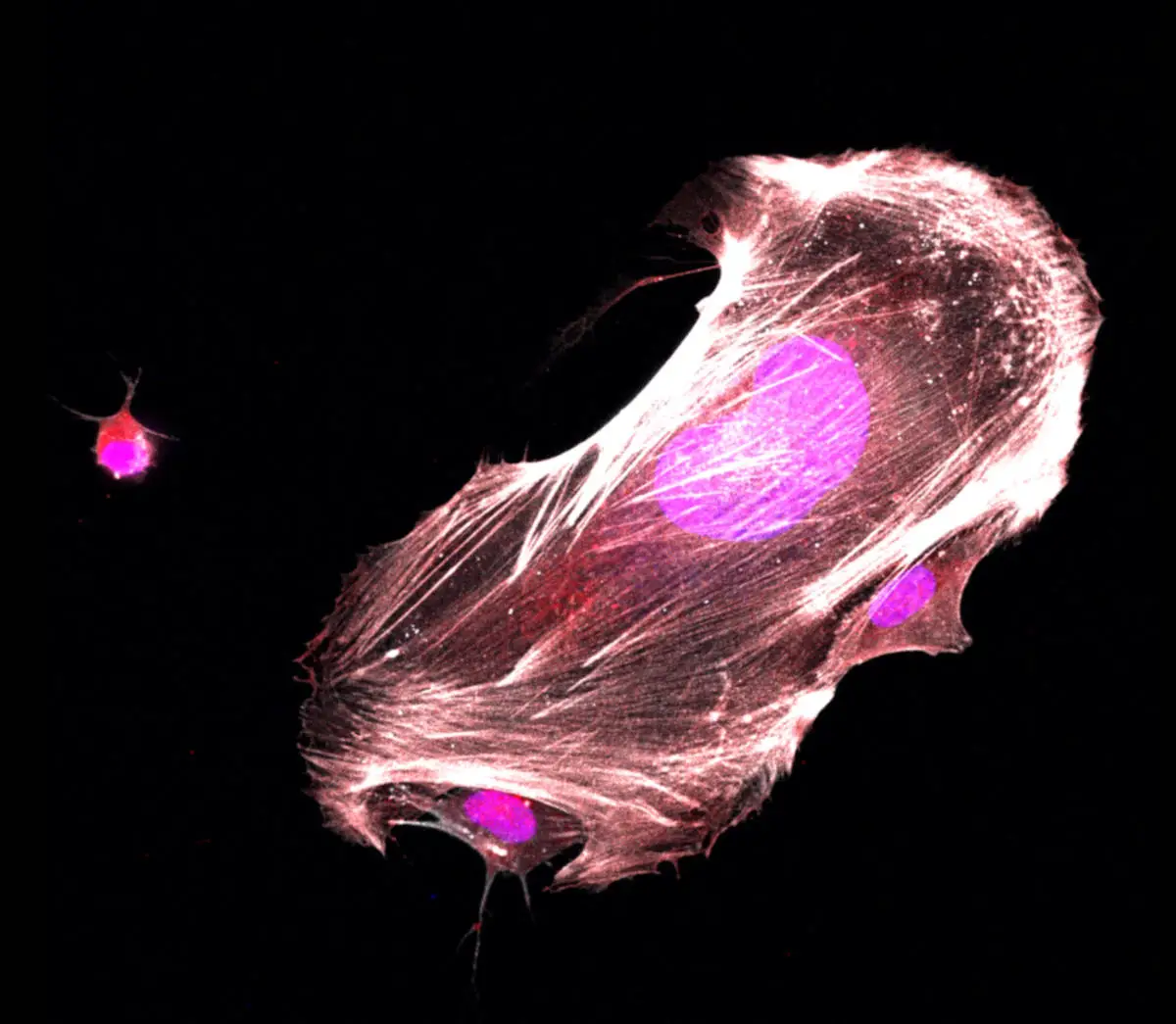
When IRE1α is triggered in cells undergoing stress, it starts producing XBP1s, a multitasking transcription factor that controls the expression of diverse gene programs in a context-specific manner. The researchers analyzed the expression levels of the gene encoding XBP1s from a large set of human NSCLC samples cataloged in a national database and found evidence that patients whose tumors had higher XBP1s levels had worse chances of survival. Consistent with that finding, they showed that knocking out IRE1α or XBP1s in NSCLC-like tumors in mice led to tumor regression and markedly improved survival.
Further investigation revealed that the deletion of XBP1s in NSCLC cells impairs tumor growth mainly by allowing the immune system to attack the tumor much more effectively. The scientists found that XBP1s, when produced within tumor cells, increases the production of a strongly immunosuppressive molecule called prostaglandin E2, which is secreted into the tumor microenvironment where it effectively suppresses the anticancer activity of immune cells.
The findings suggest that disabling IRE1α-XBP1s might be a good treatment strategy for NSCLC and might work particularly well in combination with other immunotherapy approaches.
Mapping the Gene Activity Signature
As part of the study, the