Summary of A Simple Blood Protein Could Transform Treatment of a Deadly Fungal Disease:
Recent research has highlighted albumin, the most prevalent protein in human blood, as a critical protector against mucormycosis, an aggressive fungal infection linked to high mortality rates. Conducted by an international team led by Dr. George Chamilos and Dr. Ashraf Ibrahim, the study published in Nature finds that lower levels of albumin, known as hypoalbuminemia, are strongly associated with poor patient outcomes, indicating a potential biomarker for identifying those at risk.
The findings suggest that therapies aimed at increasing albumin levels could prevent the infection, particularly in vulnerable populations affected during the COVID-19 pandemic. The research demonstrates that albumin inhibits the growth of Mucorales fungi while leaving other microbes unharmed, suggesting a promising avenue for new preventive and treatment strategies against this life-threatening disease.
*****
Summary Bullet Points
- Albumin’s Role: Researchers have discovered that albumin, the most abundant protein in human blood, plays a crucial defense role against mucormycosis, a lethal fungal infection.
- Hypoalbuminemia: Low levels of albumin (hypoalbuminemia) have been identified as key indicators of poor outcomes for patients with mucormycosis, indicating a higher risk for serious progression of the disease.
- Mechanism of Action: Albumin works to inhibit the growth and virulence of Mucorales fungi, disrupting their metabolism and protecting human tissues.
- Potential Therapies: The findings suggest that albumin-based therapies could be developed to prevent and treat mucormycosis, offering hope for patients with limited options.
- Future Research: Ongoing research aims to explore combination therapies that pair albumin with immunotherapies targeting the pathogens responsible for this formidable disease.
A Simple Blood Protein Could Transform Treatment of a Deadly Fungal Disease
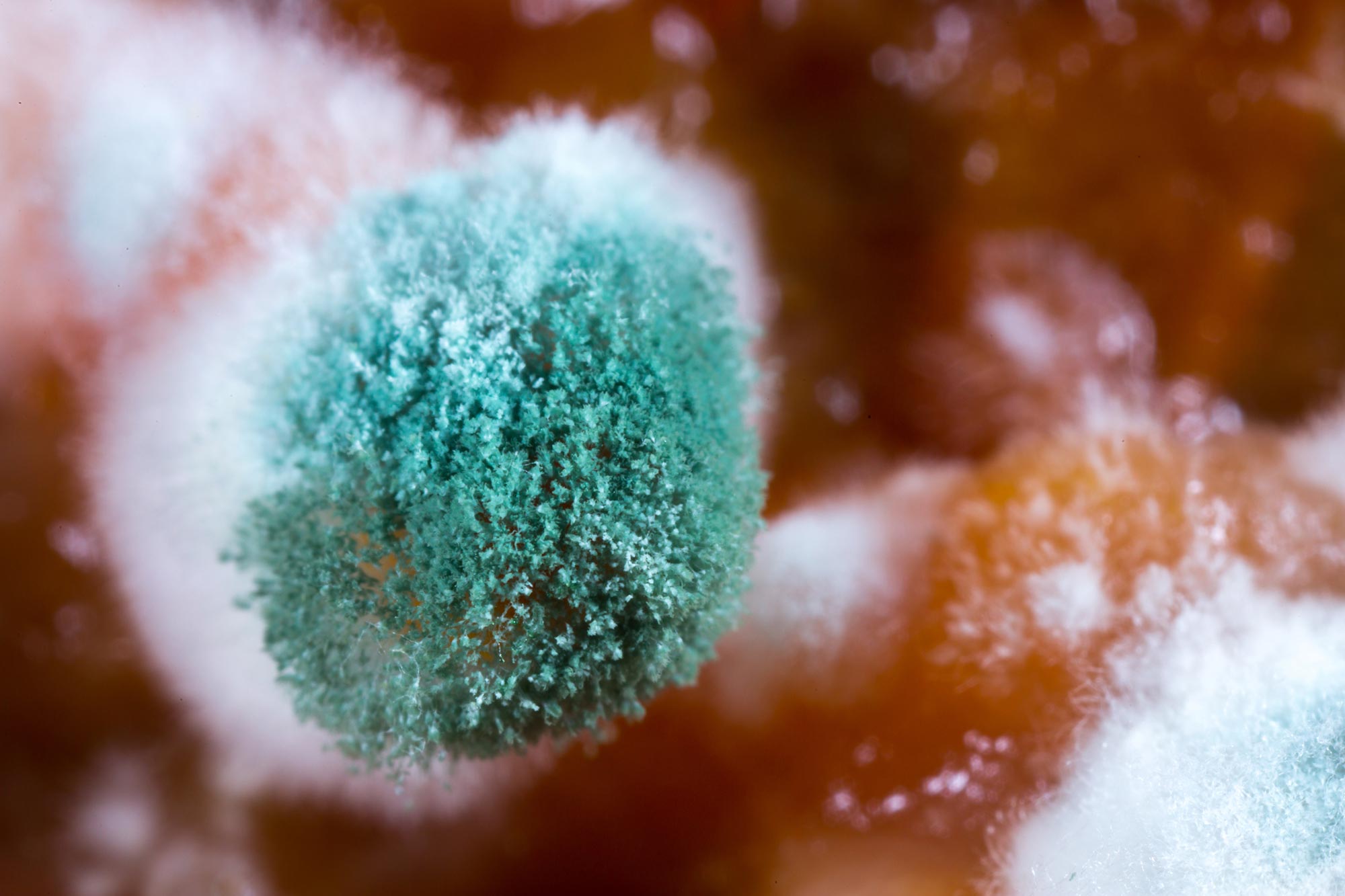
Imagine a world where a simple protein found in your blood could dramatically alter the landscape of treatment for one of the most aggressive and potentially deadly infections known to medicine. This scenario is closer to reality than one might think, thanks to groundbreaking research highlighting the role of albumin in countering the vicious effects of mucormycosis, often deemed “black fungus.”
The Unfolding Drama of Mucormycosis
To grasp the significance of this discovery, one must first understand the grave nature of mucormycosis. This infection, initiated by a group of fungi known as Mucorales, can erupt swiftly and lead to fatal consequences. Its association with other conditions—such as diabetes, malnutrition, and compromised immune systems—has garnered international attention, particularly during the COVID-19 pandemic when its prevalence surged, particularly in certain vulnerable populations, such as those in India. The disease is astonishingly lethal, with mortality rates reaching 50% or even more in acute cases.
Discovering the Hidden Defender: Albumin
Researchers from the University of Crete and the Lundquist Institute for Biomedical Innovation have embarked on a journey that reveals a surprising link between albumin levels in the blood and the severity of mucormycosis. Albumin, the most abundant protein in human plasma, has now taken center stage as a formidable ally in our defense against infections. Their studies unveiled a striking pattern: patients with mucormycosis consistently exhibited lower levels of albumin compared to those suffering from other fungal infections. This phenomenon, known as hypoalbuminemia, has emerged as a powerful predictor of adverse outcomes in affected individuals.
Dr. Ashraf Ibrahim, a leading figure in this research, emphasized the transformative potential of this finding. If clinicians can identify at-risk patients through albumin levels, preventive measures can be deployed, possibly averting the onset of this deadly disease altogether. Imagine patients receiving albumin infused with free fatty acids—an approach that could serve as a cutting-edge treatment strategy tailored to shield them from mucormycosis.
How Does Albumin Work?
As you delve deeper into the scientific intrigue, a question arises: how exactly does this protein exert its protective effects? According to researchers, albumin plays a critical role not merely by being present in the bloodstream but actively engaging in neutralizing several virulence factors of the Mucorales fungus. Consider this: albumin has the ability to bind with fatty acids, which then disrupt the metabolic functions of the fungus. This inhibition hampers the pathogen’s invasion strategies and its ability to wreak havoc on healthy human tissues.
In a telling experiment, scientists removed albumin from blood samples, allowing the Mucorales fungi to flourish unrestricted, demonstrating the protein’s pivotal role as a suppressant against this dangerous pathogen. Furthermore, in animal models devoid of albumin, researchers witnessed a horrifying susceptibility to infection, in stark contrast to those with normal albumin levels, who exhibited a fortified defense.
A New Path for Prevention
The discovery of albumin’s protective qualities unveils a powerful new narrative in the realm of infectious disease management. With current treatments for mucormycosis being limited and often inadequate, this fresh understanding offers precious hope. As Dr. Ibrahim explained, the identification of hypoalbuminemia as a potential biomarker opens up avenues for early intervention, allowing healthcare providers to enact preventive treatments in high-risk populations.
This paradigm shift propels medical practitioners to consider innovative approaches that mix traditional therapies with novel albumin-based formulations. Effective treatment of mucormycosis may not be a distant goal but rather an imminent breakthrough awaiting implementation in clinical settings.
The Future is Bright
Imagine walking into a clinic where a simple blood test for albumin levels could not only offer insights into your health but also transform how your medical care is tailored. Empowering patients with knowledge and actionable interventions is a paramount goal in the medical community, and the prospect of albumin-based therapies for mucormycosis aligns perfectly with this ethos.
Moreover, this research paves the way for further studies focusing on merging albumin treatments with immunotherapies aimed at eradicating Mucorales virulence factors. The potential for synergy between these treatment modalities hints at an optimistic future for those at risk.
Completion of the Circle
The advent of this research goes beyond mere science; it embodies the inexorable link between understanding our bodies and leveraging that understanding for better health outcomes. Just as cells and proteins communicate within us, this research establishes a dialogue between science and clinical practice, urging us to appreciate the nuances of our biological systems.
Discerning the delicate balance between health and disease opens gateways to exploration—reminding us that every protein, every enzyme, and every chemical in our bodies holds keys to mysteries yet unsolved. The narrative surrounding albumin is merely a slice of a much larger story that humanity is writing.
A Call to Learning and Discovery
As new findings emerge, it is imperative to remain curious and engaged. We must advocate for continued research and support efforts aimed at better understanding both the mechanisms of disease and the avenues for treatment. This journey is not solely the responsibility of researchers; rather, it involves all of us. By staying informed, sharing knowledge, and participating in discussions, we can contribute to a future brimming with hope and innovation.
This complex saga illustrates the significance of collaboration—the merging of minds across borders, disciplines, and specialties working together to combat formidable challenges in healthcare.
Conclusion
In closing, the relationship between albumin and mucormycosis is a testament to how even the most commonplace elements of our biology can yield extraordinary insights. Each breakthrough—not just in the lab but also in the world of clinical practice—brings us closer to that transformative future where disease management is not just reactive, but proactive.
As we stand on the precipice of new medical frontiers, the allure of science and its potential to enhance human existence continues to inspire generations. The path forward is laden with possibilities, and with each discovery, we inch closer to the ultimate goal: a healthier world for all.
Stay curious, stay invested, and let the story of albumin and its protective power against mucormycosis be a reminder that hope often hides in the most unexpected places.