Summary of Cocaine Addiction Makes the Brain Age Faster – Could Be Caused by Inflammation or Cell Death:
In this study, researchers from Germany and Canada have found that cocaine use disorder (CUD) causes alterations in the “methylome” of Brodmann Area 9, a subregion within the prefrontal cortex, which is responsible for self-awareness and inhibitory control. The study, published in Frontiers in Psychiatry, found that an increased level of DNA methylation is associated with the suppression of neighboring genes, as well as evidence that cells in Brodmann Area 9 appear biologically ‘older’ in people with CUD than in those without CUD. They also found 17 genomic regions that were more methylated in donors with CUD than in donors without CUD, and three regions that were less methylated in donors with CUD than in donors without CUD. These findings suggest that cocaine use disorder leads to changes in the methylome of the prefrontal cortex, which may contribute to the associated behavioral aspects of addiction.
*****
Cocaine Use Disorder Causes Changes in Prefrontal Cortex DNA Methylation
Cocaine use disorder (CUD) causes alterations in the “methylome” of Brodmann Area 9, a subregion within the prefrontal cortex, which is responsible for self-awareness and inhibitory control. This is according to a study conducted by researchers from Germany and Canada and published in Frontiers in Psychiatry. An increased level of DNA methylation is associated with the suppression of neighboring genes.
Researchers discover differences in DNA methylation inside brain region important for inhibitory control in people with cocaine use disorder.
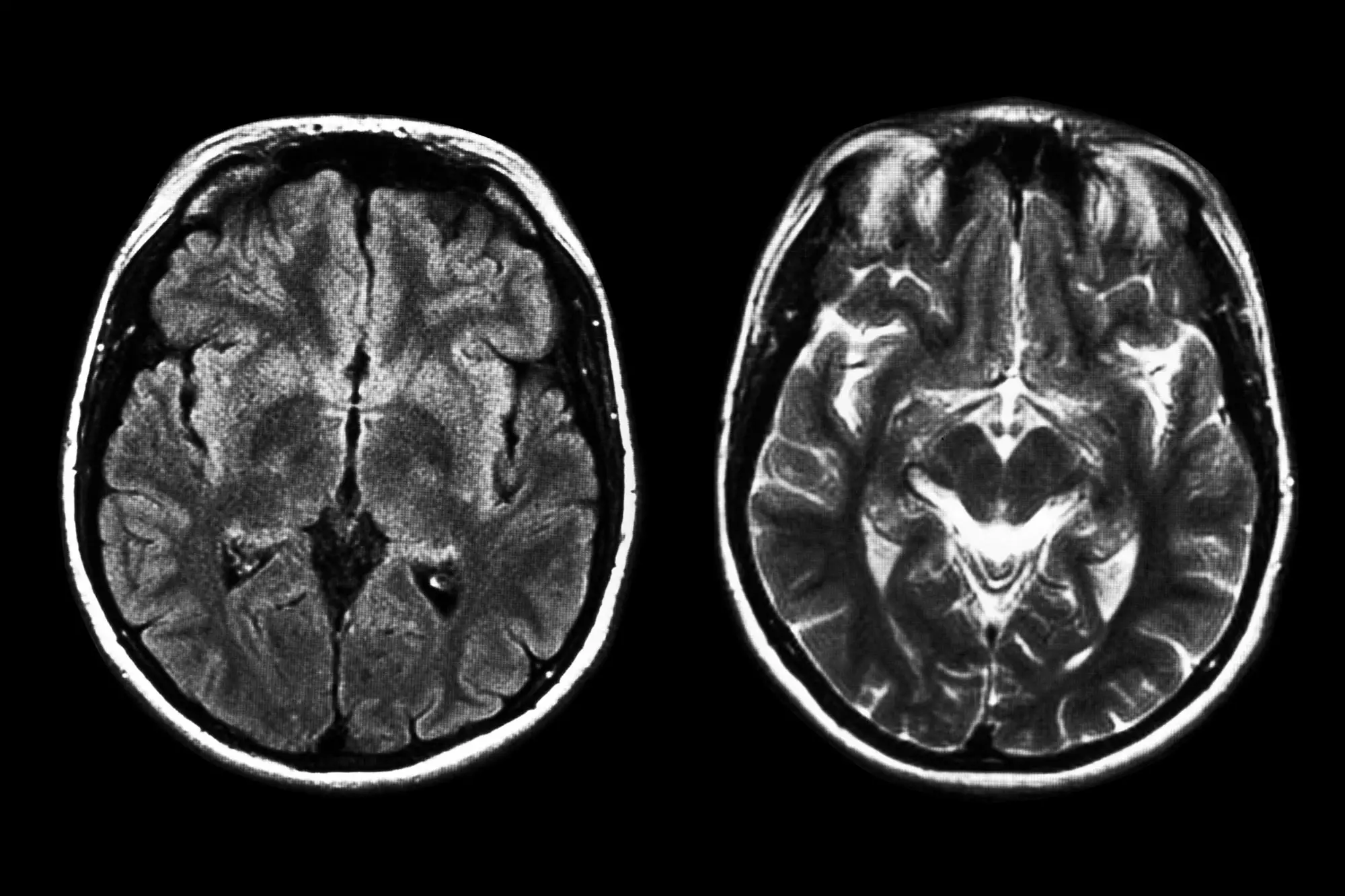
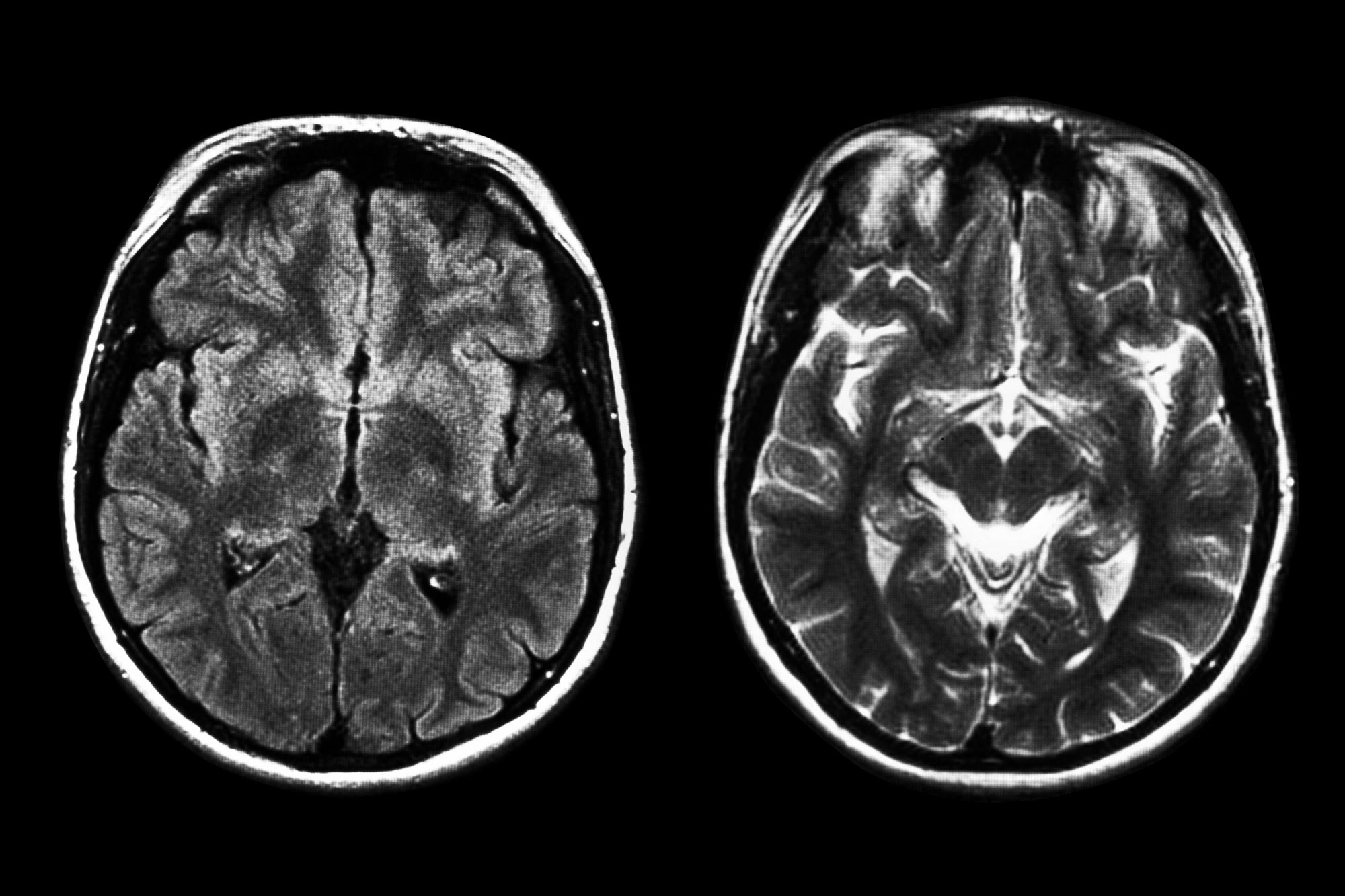
Scientists tend to view substance addiction as primarily a disease of the brain. When we enjoy sex, food, music, or hobbies, regions of our brain within the reward pathway are flooded with pleasure-inducing dopamine. Drugs like cocaine copy this effect, except up to ten times more strongly. Healthy brains aren’t at the mercy of such dopamine rushes, however: there, the prefrontal cortex weighs options and can decide to forego pleasurable activities when it’s not the time or place. In contrast, such ‘inhibitory control’ is impaired in the addicted brain, making it hard to resist. But what are the biochemical changes in the prefrontal cortex that cause this impairment?
“We detected a trend towards stronger biological aging of the brain in individuals with cocaine use disorder compared to individuals without cocaine use disorder. This could be caused by cocaine-related disease processes in the brain, such as inflammation or cell death.” — Dr. Stephanie Witt
Now, in the journal Frontiers in Psychiatry, scientists from Germany and Canada have shown that in humans, cocaine use disorder (CUD) leads to changes in the ‘methylome’ of a subregion within the prefrontal cortex, Brodmann Area 9, thought to be important for self-awareness and inhibitory control. Typically, a greater degree of DNA methylation leads to the ‘dialing down’ of nearby genes.
“As DNA methylation is an important regulatory mechanism for gene expression, the identified DNA methylation alterations might contribute to functional changes in the human brain and thereby to the associated behavioral aspects of addiction,” said first author Eric Poisel, a PhD student at the Central Institute of Mental Health in Mannheim, Germany.
Because the study of the brain methylome is invasive, the study was done on the cryo-preserved brains of 42 deceased male donors, of whom half had had CUD while the other half had not. This is important, because most earlier studies in this field were done on the brains of rats.
Brain cells may age faster in people addicted to cocaine
The researchers found evidence that cells in Brodmann Area 9 appear biologically ‘older’ in people with CUD, evidence that these cells age faster than in people without substance use disorders. Here, they used patterns of DNA methylation as a measure of the biological age of cells in Brodmann Area 9. The biological age of cells, tissues, and organs can be greater or less than their chronological age, depending on diet, lifestyle, and exposure to disease or harmful environmental factors. Scientists can thus estimate the biological age from methylome data with established mathematical algorithms.
“We detected a trend towards stronger biological aging of the brain in individuals with cocaine use disorder compared to individuals without cocaine use disorder. This could be caused by cocaine-related disease processes in the brain, such as inflammation or cell death,” said lead author Dr. Stephanie Witt, a researcher at the same institute.