Summary of Scientists Turn Cancer’s Bodyguards Against It:
Researchers at Mount Sinai have developed a novel immunotherapy to combat metastatic cancer by targeting tumor-associated macrophages, which typically protect cancer cells. Instead of attacking the cancer cells directly, this therapy disables these macrophages to allow the body’s immune system to penetrate tumors more effectively. The approach, inspired by a “Trojan horse” strategy, uses engineered CAR T cells designed to recognize and eliminate these protective macrophages. Initial preclinical trials in lung and ovarian cancer models showed promising results, increasing survival rates and potentially reshaping the tumor environment to allow for greater immune activity. While the findings are encouraging, further studies are necessary to evaluate safety and effectiveness in humans.
*****
Summary Bullet Points
- Researchers have developed an innovative immunotherapy that targets tumor-associated macrophages, easing access for the immune system to attack cancer cells.
- The process involves using engineered CAR T cells that can shift macrophages from protective roles to offensive ones against tumors.
- This therapy aims to reshape the tumor microenvironment to become more immune-active, potentially creating broader applications across various cancer types.
- The results show promising preclinical outcomes in mice with metastatic ovarian and lung cancer, with many animals experiencing extended lifespans or complete cures.
- While preliminary, the research represents a significant step toward new cancer treatments, emphasizing the importance of turning tumor "guards" into "allies."
Transforming Cancer’s Bodyguards into Weapons Against It
Imagine standing in front of a fortress—strong, intimidating, and seemingly impenetrable. Inside, however, lie treasures waiting to be discovered. In the complex world of cancer biology, the fortress represents tumors, while the guards are specialized immune cells known as macrophages. A groundbreaking study from the Icahn School of Medicine at Mount Sinai reveals a dramatic shift in how we can approach cancer treatment, flipping the script on conventional immunotherapy.
The Trojan Horse Approach
To understand this research, we must first acknowledge the limitations of traditional cancer therapies. Conventional methods often focus on attacking the cancer cells directly. It’s straightforward, right? However, tumors are cunning; they erect protective barriers to shield themselves from these attacks—transforming supportive immune cells into unsuspecting allies in their defense.
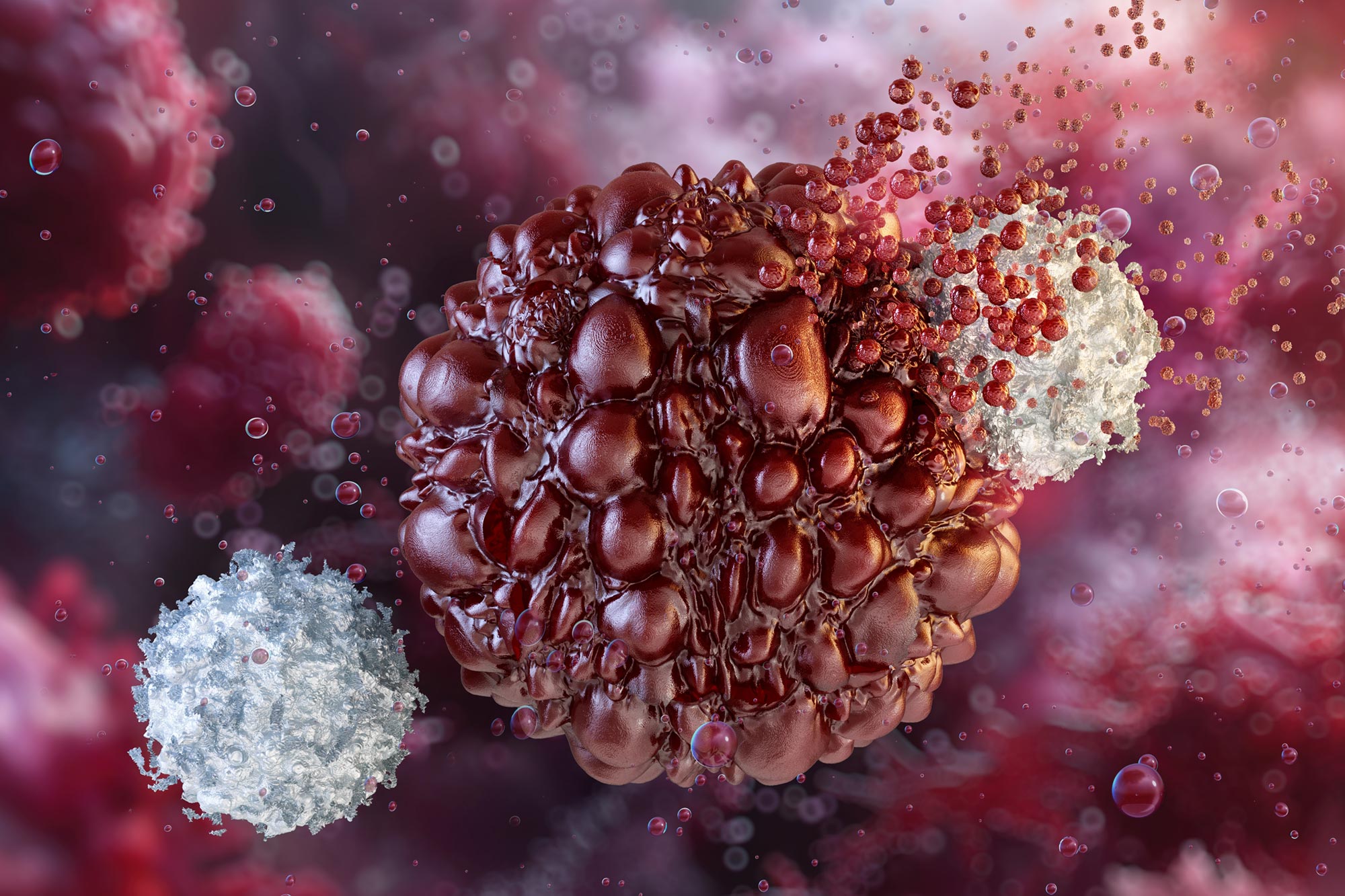
This is where the Trojan horse analogy comes into play. The researchers decided to circumvent direct confrontation and instead targeted the protective macrophages that surround the cancer cells. By disabling these immune bodyguards, they created a path for the immune system to penetrate the tumor’s defenses and unleash its full force.
So, what do macrophages have to do with cancer? Normally, these cells act as defenders, constantly monitoring and responding to threats. In the presence of tumors, they often change roles, becoming unwitting accomplices to cancer’s growth and spread. Researchers at Mount Sinai realized that to defeat the fortress, they had to first turn the guards on their heads—and this is effectively what they set out to do.
The Science of Marcrophages
The study introduces a fascinating dimension to cancer therapy: the manipulation of tumor-associated macrophages. In a typical scenario, these immune cells respond effectively to pathogens, cleaning up debris and facilitating healing. However, inside the tumor microenvironment, they undergo a transformation, morphing into agents that block immune defenses.
Jaime Mateus-Tique, the study’s lead author, refers to tumors not merely as clusters of malignant cells but as intricate ecosystems where these cells thrive, relying heavily on their macrophage bodyguards for protection. Their research set the ambitious goal of converting these guards from protectors of the tumor into agents of its demise.
This innovative spirit is at the heart of modern scientific discovery: to see beyond the obvious and explore creative avenues.
CAR T Cells Reimagined
Engineered T cells, known as CAR T cells, have gained notoriety for their role in directly targeting and destroying cancer cells. However, not every kind of cancer displays clear “marks” that these cells can identify. This presents a significant hiccup in treating solid tumors where traditional cancer markers remain elusive.
Mount Sinai’s research ingeniously redirected CAR T cells to instead identify and engage the reformulated macrophages that were previously supporting the tumor. The researchers designed these cellular warriors to release interleukin-12, an immune-boosting molecule that activates other immune cells, particularly killer T cells. Through this line of attack, they aimed to initiate an immune response that can dismantle the protective layers of the tumor.
When tested in aggressive preclinical models of metastatic lung and ovarian cancer, the results were nothing short of remarkable. Mice treated with the engineered CAR T cells lived significantly longer. Some were given a second chance at life—experiencing what could only be described as complete cures. It’s a powerful reminder of how ingenuity and collaboration can yield extraordinary results.
Shaping the Tumor Microenvironment
Why is this reconfiguration of the tumor environment essential? Essentially, it transforms a garden of suppression into one of action. The treatment reshaped the tumor’s biological landscape, allowing for immune cells capable of attacking and eradicating cancer to swarm into the space previously governed by mixed messages of persisting immune suppression.
Employing advanced spatial genomics techniques, the researchers monitored these changes closely, observing a remarkable reduction in immune-suppressing cells and a concurrent influx of immune responders ready to battle cancer. This innovative therapy highlighted the groundbreaking potential of being "antigen-independent," thereby opening doors for broader applications across various cancers.
This is where the beauty of scientific progress shines: when one door closes, often multiple pathways emerge, creating avenues for treatments where once there were none.
Implications for Future Therapies
It’s important to outline that the journey isn’t over. The researchers themselves express cautious optimism, emphasizing the need for human studies to assess safety and efficacy. However, the findings mark a significant leap in cancer treatment strategies, holding profound implications for how various cancers respond to therapy.
Dr. Brian Brown, one of the study’s senior authors, encapsulated this excitement, stating that their treatment pivots from merely attacking cancer cells to fundamentally altering the environment in which these cells exist. The team continues to refine the therapy, focusing on the optimal release of interleukin-12 within tumors to maximize anti-cancer effects while safeguarding patient safety.
The excitement surrounding this discovery is palpable. If successful in clinical applications, it wouldn’t just be another treatment but perhaps a new paradigm in cancer therapy. Instead of targeting cancer cells alone, future therapies may simultaneously focus on dismantling the cohorts that shield tumors, transforming the overall approach to treatment.
What Lies Ahead
As we embrace this new knowledge, the horizon of cancer therapy appears more promising. The dual focus on cancer and its protective environment could potentially pave the way for more effective treatments across a spectrum of conditions.
Each step taken in this research is a reminder: science is not a straight path but a meandering journey filled with unexpected twists, false starts, and, ultimately, breakthroughs. With every lesson learned, we edge closer to a day when battling cancer could involve not just brute force but strategic finesse—turning the enemy’s own defenses into the frontline of attack.
It’s an inspiring moment for the scientific community and for patients navigating the trials of cancer—the potential transformation of treatment philosophies and the promise of hope.
Final Thoughts
In the face of such formidable challenges, we find strength in collaboration and creativity. The Mount Sinai study highlights the profound impact of thinking differently, encouraging a collective re-imagining of longstanding paradigms. As technology advances and our understanding of cancer deepens, this journey teaches us that in fragmentation also lies opportunity. Just as the researchers flipped the battlefield dynamics, we, too, can flip the narratives in our lives.
Let this groundbreaking discovery inspire each of us. Whether facing personal battles or collective challenges, there is always a means to adapt, overcome, and innovate—transforming obstacles into pathways for growth and healing. Science teaches us to be resilient, to reset perspectives, and to forge powerful connections, embodying the spirit of unity, creativity, and unwavering hope.